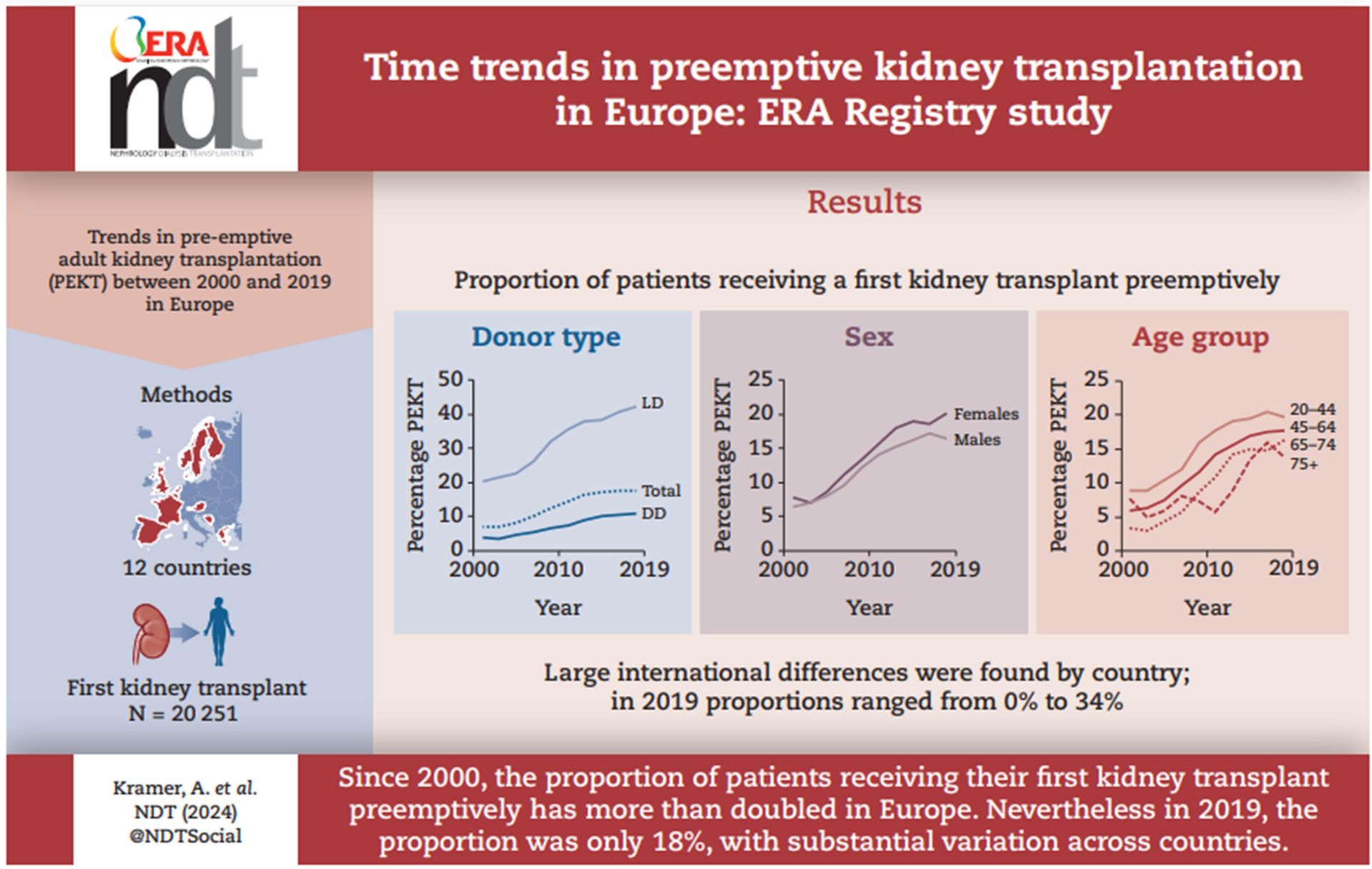
Methodology and study design
Major findings
Theoretical and practical implications
Study limitations and future research
Conclusion
Link to published article
Definitions of technical terms
- Pre-emptive Kidney Transplantation (PEKT): Transplanting a kidney into a patient before they need dialysis.
- Nephrology: The medical field focused on kidney health and diseases.
- Joinpoint regression analysis: Joinpoint regression analysis is a statistical method used to identify points where a significant change in the trend of a data series occurs. It models data as a series of linear segments joined at these "joinpoints," allowing for the detection of shifts in trends, such as changes in the rate of increase or decrease over time. This method is commonly used in epidemiology, economics, and other fields to analyse trends and determine when and where significant changes have taken place.
References
- Azegami T, Kounoue N, Sofue T, et al. Efficacy of pre-emptive kidney transplantation for adults with end-stage kidney disease: a systematic review and meta-analysis. Ren Fail 2023;45(1):2169618.
- Gill JS, Rose C, Joffres Y, et al. Variation in Dialysis Exposure Prior to Nonpreemptive Living Donor Kidney Transplantation in the United States and Its Association With Allograft Outcomes. Am J Kidney Dis 2018;71(5):636-647.
- Phongphithakchai A, Phisalprapa P, Kositamongkol C, et al. Preemptive Living-Related Kidney Transplantation Is a Cost-Saving Strategy Compared With Post-dialysis Kidney Transplantation in Thailand. Front Med (Lausanne) 2022;9:869535.
- Boenink R, Astley ME, Huijben JA, et al. The ERA Registry Annual Report 2019: summary and age comparisons. Clin Kidney J 2022;15(3):452-472.
- UK Renal Registry: UK Renal Registry 24th Annual Report, Chapter 2: Adults starting kidney replacement therapy (KRT) for end-stage kidney disease (ESKD) in the UK in 2020. Bristol, UK, 2022. Available at: https://ukkidney.org/audit-research/annual-report.
- Abecassis M, Bartlett ST, Collins AJ, et al. Kidney transplantation as primary therapy for end-stage renal disease: a National Kidney Foundation/Kidney Disease Outcomes Quality Initiative (NKF/KDOQITM) conference. Clin J Am Soc Nephrol 2008;3(2):471-480.
- Waterman AD, Morgievich M, Cohen DJ, et al. Living Donor Kidney Transplantation: Improving Education Outside of Transplant Centers about Live Donor Transplantation--Recommendations from a Consensus Conference. Clin J Am Soc Nephrol 2015;10(9):1659-1669.
- Kallab S, Bassil N, Esposito L, et al. Indications for and barriers to preemptive kidney transplantation: a review. Transplant Proc 2010;42(3):782-784.
- Joinpoint Regression Program, Version 4.2.0.2. June 2015; Statistical Research and Applications Branch, National Cancer Institute.
- Kim HJ, Fay MP, Feuer EJ, et al. Permutation tests for joinpoint regression with applications to cancer rates. Stat Med 2000;19(3):335-351.
- SAS software, Version 9.4. Copyright ©. SAS Institute Inc., Cary, NC, USA.
- Berthoux FC, Jones EH, Mehls O, et al. Transplantation Report. 2: Pre-emptive renal transplantation in adults aged over 15 years. The EDTA-ERA Registry. European Dialysis and Transplant Association-European Renal Association. Nephrol Dial Transplant 1996;11 Suppl 1:41-43.
- Kasiske BL, Snyder JJ, Matas AJ, et al. Preemptive kidney transplantation: the advantage and the advantaged. J Am Soc Nephrol 2002;13(5):1358-1364.
- Meier-Kriesche HU, Kaplan B. Waiting time on dialysis as the strongest modifiable risk factor for renal transplant outcomes: a paired donor kidney analysis. Transplantation 2002;74(10):1377-1381.
- Davis CL. Preemptive transplantation and the transplant first initiative. Curr Opin Nephrol Hypertens 2010;19(6):592-597.
- Kasiske BL, Cangro CB, Hariharan S, et al. The evaluation of renal transplantation candidates: clinical practice guidelines. Am J Transplant 2001;1 Suppl 2:3-95.
- Kidney Disease: Improving Global Outcomes (KDIGO) CKD Work Group. KDIGO clinical practice guideline for the evaluation and management of chronic kidney disease. Kidney Int Suppl 2013;3:1-150.
- European Best Practice Guidelines for Renal Transplantation (part 1). Nephrol Dial Transplant 2000;15 Suppl 7:1-85.
- Boenink R, Kramer A, Tuinhout RE, et al. Trends in kidney transplantation rate across Europe: Study from the ERA Registry. Nephrol Dial Transplant 2023
- United States Renal Data System: 2022 USRDS Annual Data Report: Epidemiology of kidney disease in the United States. National Institutes of Health, National Institute of Diabetes and Digestive and Kidney Diseases, Bethesda, MD, 2022. Available at: https://usrds-adr.niddk.nih.gov/2022.
- ANZDATA Registry: 44th Report, Chapter 1: Incidence of Kidney Failure with Replacement Therapy. Australia and New Zealand Dialysis and Transplant Registry, Adelaide, Australia, 2021. Available at: http://www.anzdata.org.au.
- ANZDATA Registry: 44th Report, Chapter 7: Kidney Transplantation Australia and New Zealand Dialysis and Transplant Registry, Adelaide, Australia, 2021. Available at: http://www.anzdata.org.au.
- Pradel FG, Jain R, Mullins CD, et al. A survey of nephrologists' views on preemptive transplantation. Clin J Am Soc Nephrol 2008;3(6):1837-1845.
- Cass A, Cunningham J, Snelling P, et al. Late referral to a nephrologist reduces access to renal transplantation. Am J Kidney Dis 2003;42(5):1043-1049.
- Knight RJ, Teeter LD, Graviss EA, et al. Barriers to preemptive renal transplantation: a single center questionnaire study. Transplantation 2015;99(3):576-579.
- Dirix M, Philipse E, Vleut R, et al. Timing of the pre-transplant workup for renal transplantation: is there room for improvement? Clin Kidney J 2022;15(6):1100-1108.
- Riffaut N, Lobbedez T, Hazzan M, et al. Access to preemptive registration on the waiting list for renal transplantation: a hierarchical modeling approach. Transpl Int 2015;28(9):1066-1073.
- Fishbane S, Nair V. Opportunities for Increasing the Rate of Preemptive Kidney Transplantation. Clin J Am Soc Nephrol 2018;13(8):1280-1282.
- Maggiore U, Abramowicz D, Budde K, et al. Standard work-up of the low-risk kidney transplant candidate: a European expert survey of the ERA-EDTA Developing Education Science and Care for Renal Transplantation in European States Working Group. Nephrol Dial Transplant 2019;34(9):1605-1611.
- Formica RN, Jr., Barrantes F, Asch WS, et al. A one-day centralized work-up for kidney transplant recipient candidates: a quality improvement report. Am J Kidney Dis 2012;60(2):288-294.
- Habbous S, McArthur E, Dixon SN, et al. Initiating Maintenance Dialysis Before Living Kidney Donor Transplantation When a Donor Candidate Evaluation Is Well Underway. Transplantation 2018;102(7):e345-e353.
- Lentine KL, Kasiske BL, Levey AS, et al. KDIGO Clinical Practice Guideline on the Evaluation and Care of Living Kidney Donors. Transplantation 2017;101(8S Suppl 1):S1-s109.
- Graham JM, Courtney AE. The Adoption of a One-Day Donor Assessment Model in a Living Kidney Donor Transplant Program: A Quality Improvement Project. Am J Kidney Dis 2018;71(2):209-215.
- Purnell TS, Hall YN, Boulware LE. Understanding and overcoming barriers to living kidney donation among racial and ethnic minorities in the United States. Adv Chronic Kidney Dis 2012;19(4):244-251.
- Rodrigue JR, Cornell DL, Lin JK, et al. Increasing live donor kidney transplantation: a randomized controlled trial of a home-based educational intervention. Am J Transplant 2007;7(2):394-401.
- Ismail SY, Luchtenburg AE, Timman R, et al. Home-based family intervention increases knowledge, communication and living donation rates: a randomized controlled trial. Am J Transplant 2014;14(8):1862-1869.
- Garonzik-Wang JM, Berger JC, Ros RL, et al. Live donor champion: finding live kidney donors by separating the advocate from the patient. Transplantation 2012;93(11):1147-1150.
- Jay CL, Dean PG, Helmick RA, et al. Reassessing Preemptive Kidney Transplantation in the United States: Are We Making Progress? Transplantation 2016;100(5):1120-1127.
- Gaillard F, Jacquemont L, Roberts V, et al. Temporal trends in living kidney donation in France between 2007 and 2017. Nephrol Dial Transplant 2021;36(4):730-738.
- Salas MAP, Chua E, Rossi A, et al. Sex and gender disparity in kidney transplantation: Historical and future perspectives. Clin Transplant 2022;36(12):e14814.
- Vanholder R, Domínguez-Gil B, Busic M, et al. Organ donation and transplantation: a multi-stakeholder call to action. Nat Rev Nephrol 2021;17(8):554-568.
- Kiberd BA, Tennankore KK, Vinson AJ. Comparing the Net Benefits of Adult Deceased Donor Kidney Transplantation for a Patient on the Preemptive Waiting List vs a Patient Receiving Dialysis. JAMA Netw Open 2022;5(7):e2223325.
- Charpentier B, Durrbach A. Transplantation: pre-emptive kidney transplantation--perfect, but when? Nat Rev Nephrol 2011;7(10):550-551.
- Chadban SJ, Ahn C, Axelrod DA, et al. KDIGO Clinical Practice Guideline on the Evaluation and Management of Candidates for Kidney Transplantation. Transplantation 2020;104(4S1 Suppl 1):S11-s103.
- NHS Blood and Transplant: Patient selection for deceased donor kidney only transplantation. Bristol, UK, 2020. Available at: https://nhsbtdbe.blob.core.windows.net/umbraco-assets-corp/18170/pol184.pdf.